This is a 73 year old man who presented to his primary medical doctor with gross hematuria in 2020. He is healthy with the exception that he weighs 250 lbs with a large abdominal girth. He has not had surgery. He was a former cigarette smoker with a 30 pack years history. He stopped smoking cigarettes in 2008. He had a CT scan which was normal with the exception of thickening in the wall of the urinary bladder. A cystoscopic examination identified a large bladder tumor and he underwent a transurethral resection of the bladder tumor (TUR BT). The pathology revealed a muscle invasive urothelial carcinoma with lymphovascular invasion.
Fig. 1
Extensive resection following the initial TUR BT at another institution.
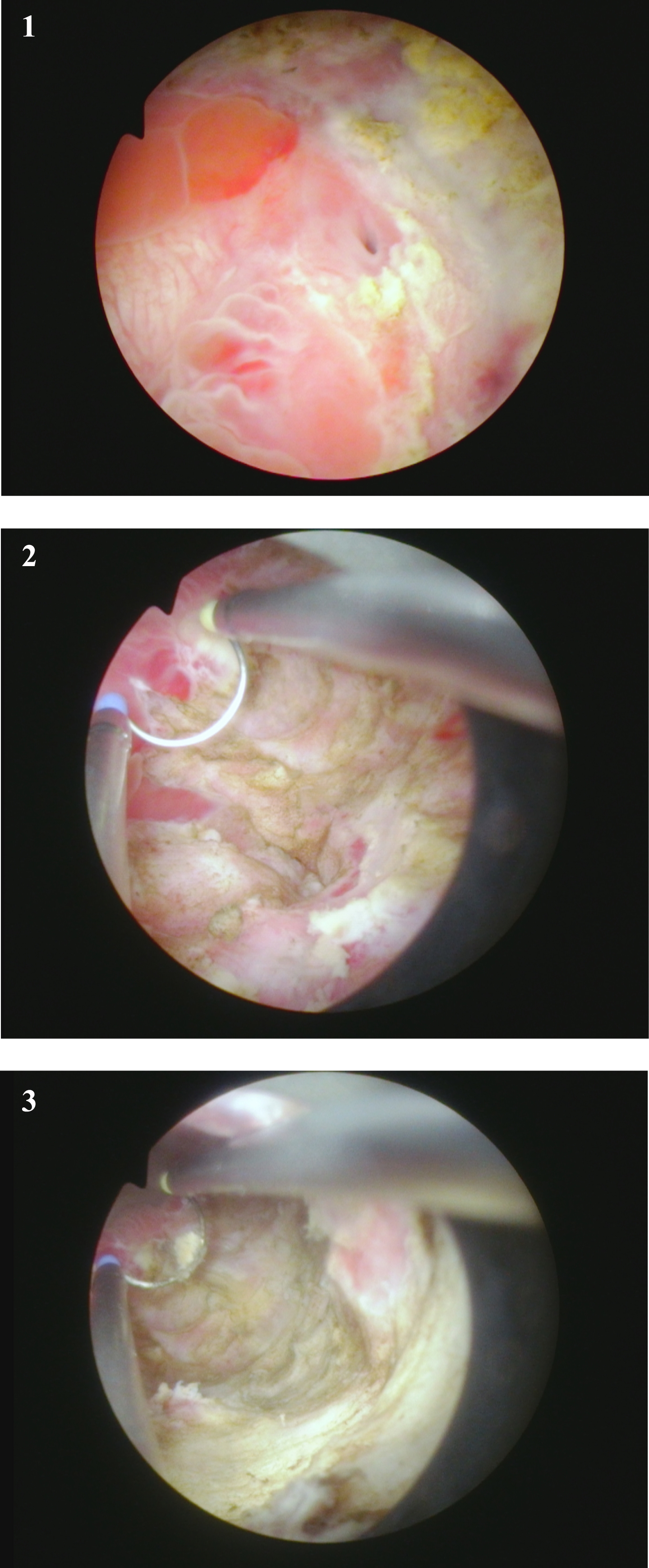
Fig. 4
Flexible cystoscopy in office identifies a large anterior exophytic bladder tumor.
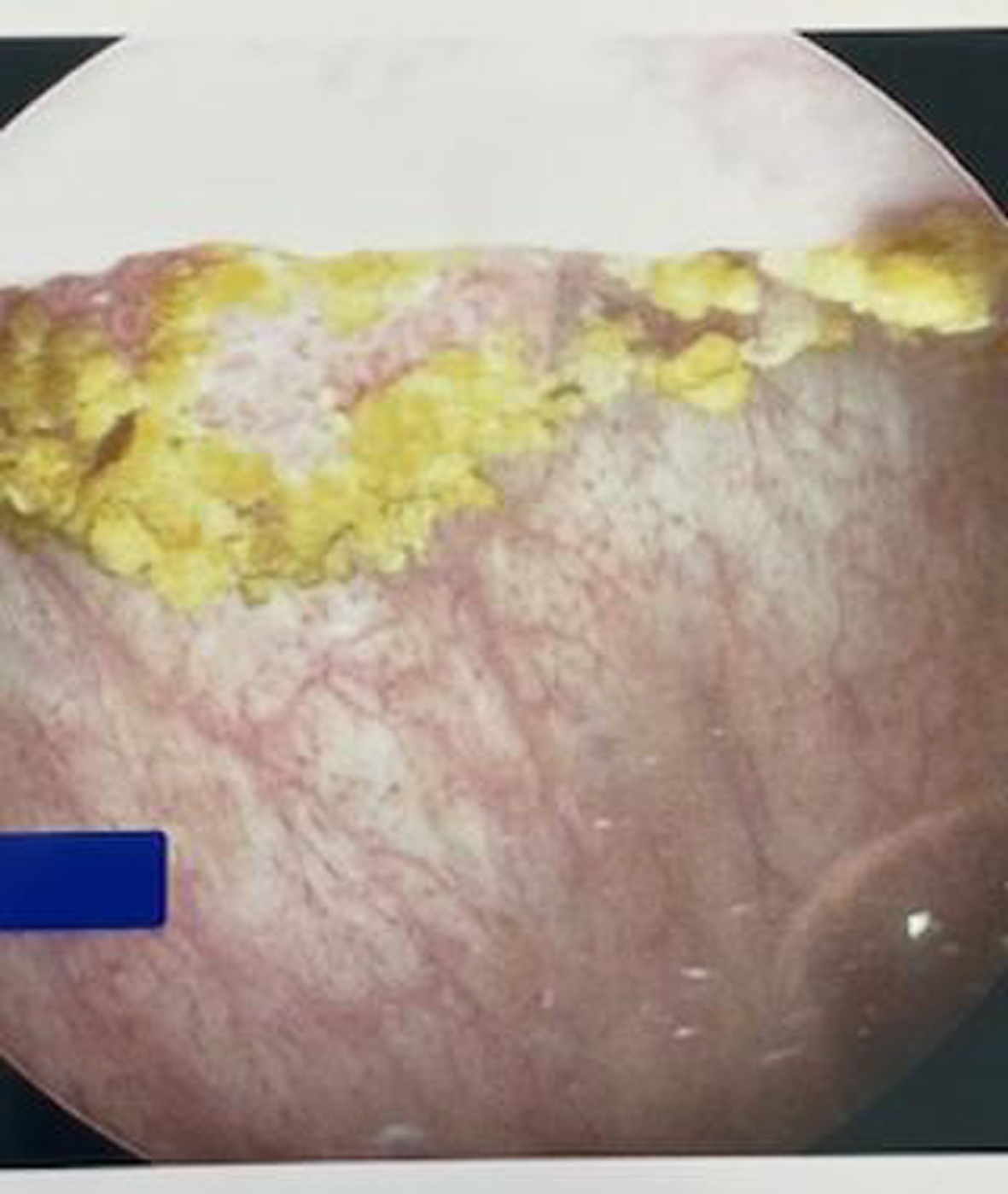
Fig. 5
CT scan indicates the tumor. There is no hydronephrosis and the bladder wall appears normal.
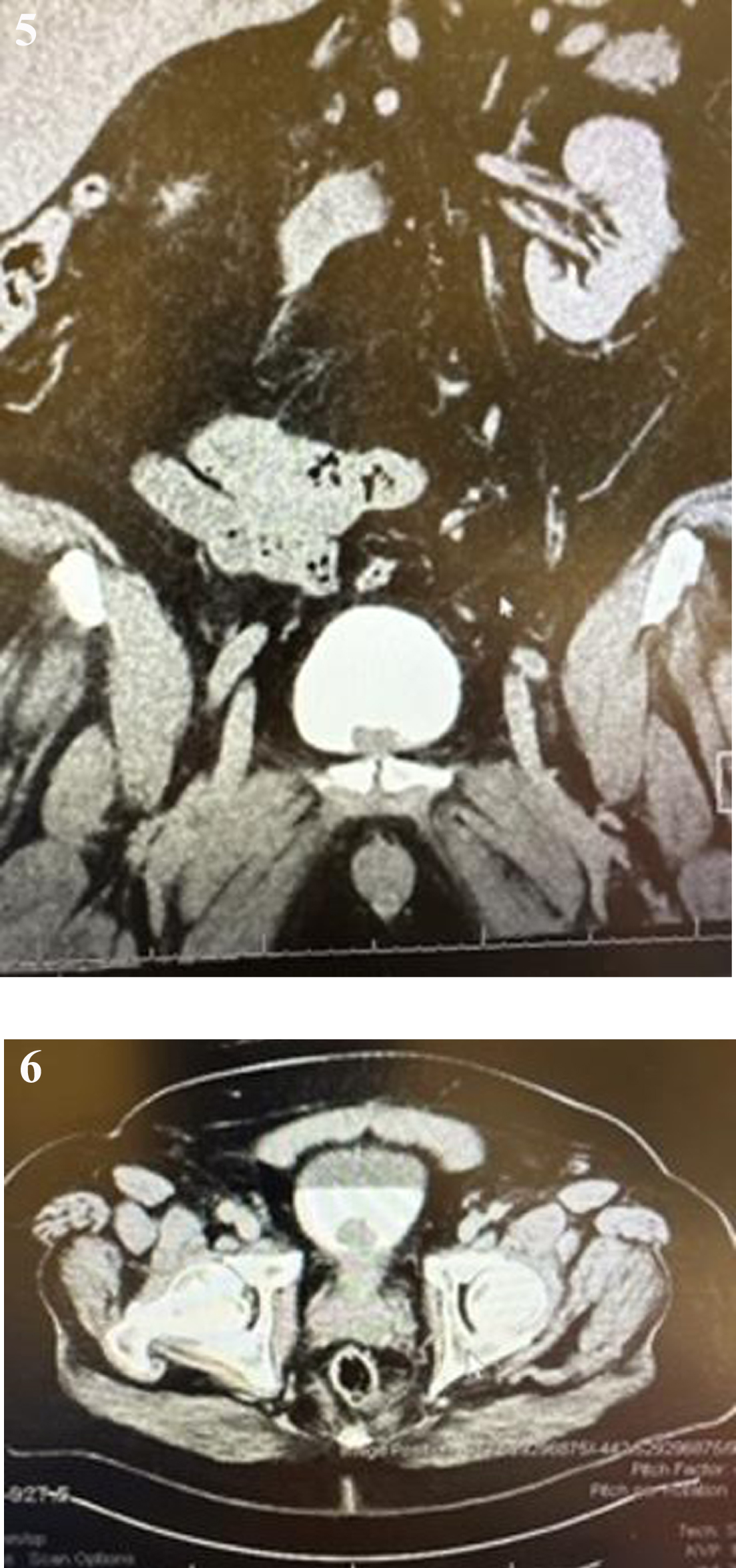
Fig. 7
Cystoscopic appearance with 70 degree lens allows visualization of some of the tumor.
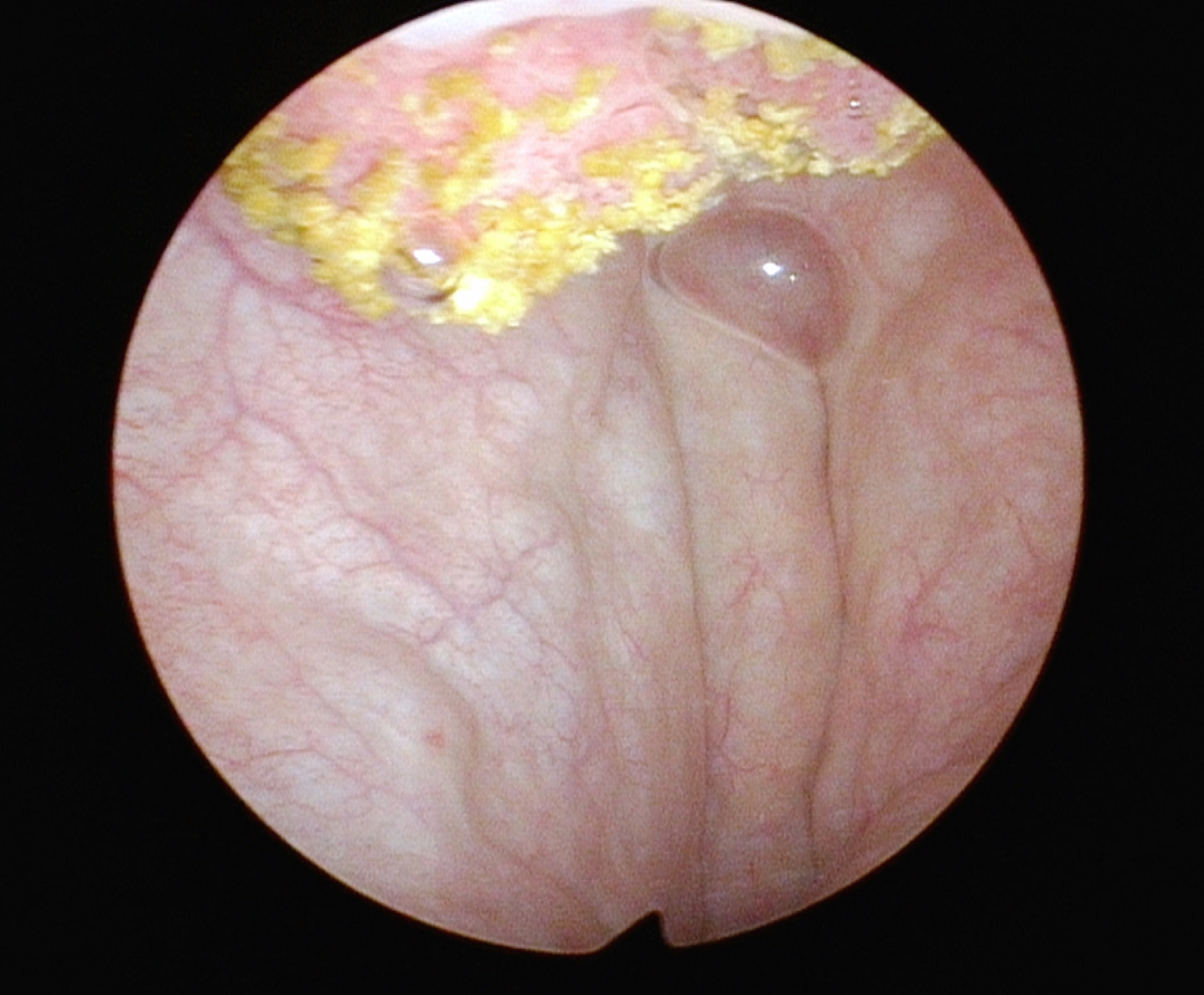
Fig. 8
Futile attempt at cautery with a bugby electrode using the 70 degree lens.
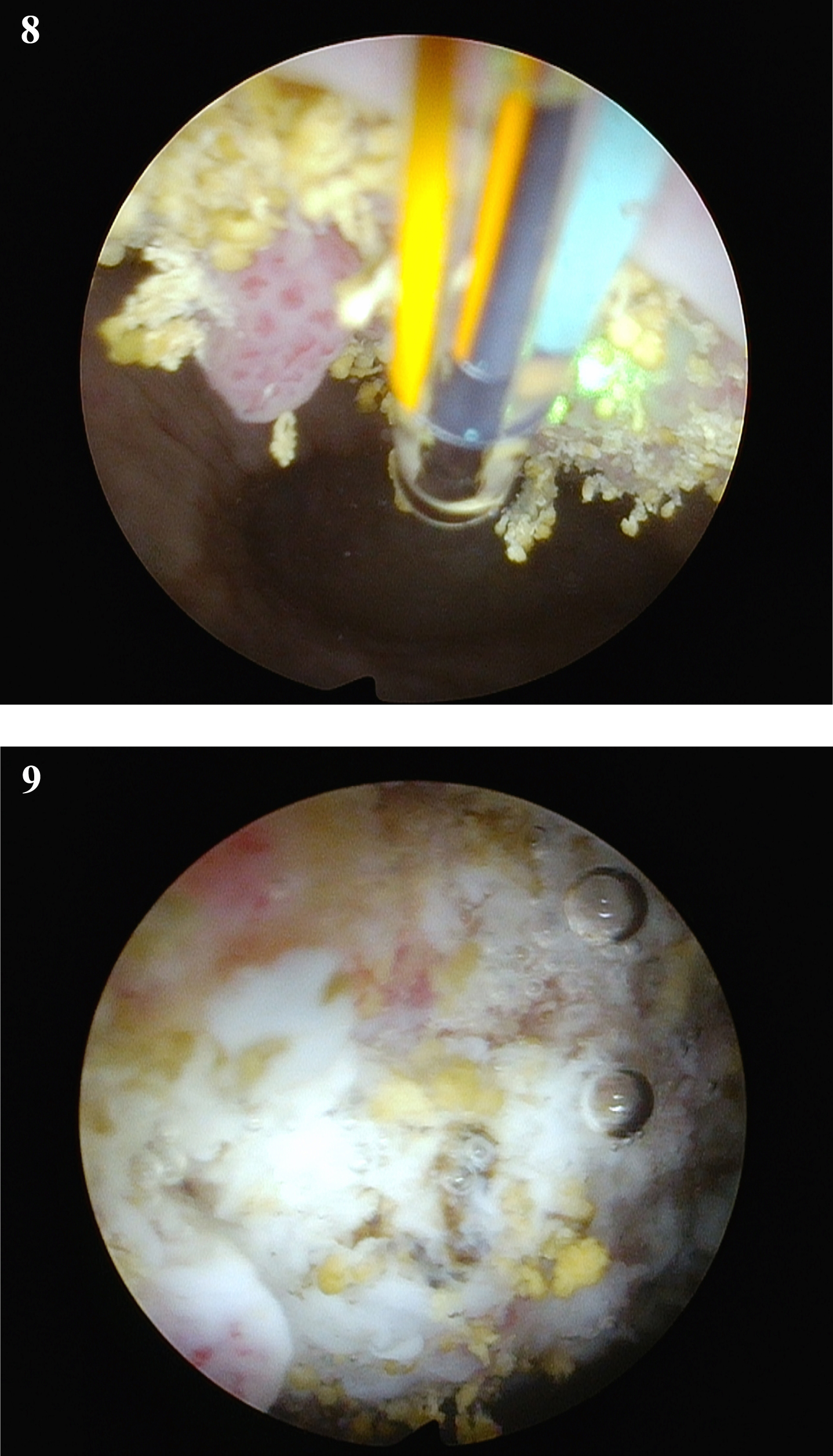
Fig. 10
Second attempt at TUR BT of anterior tumor but this time using a perineal urethrostomy which allowed visualization of the tumor with a 30 degree lens. Tumor was visibly completely resected.
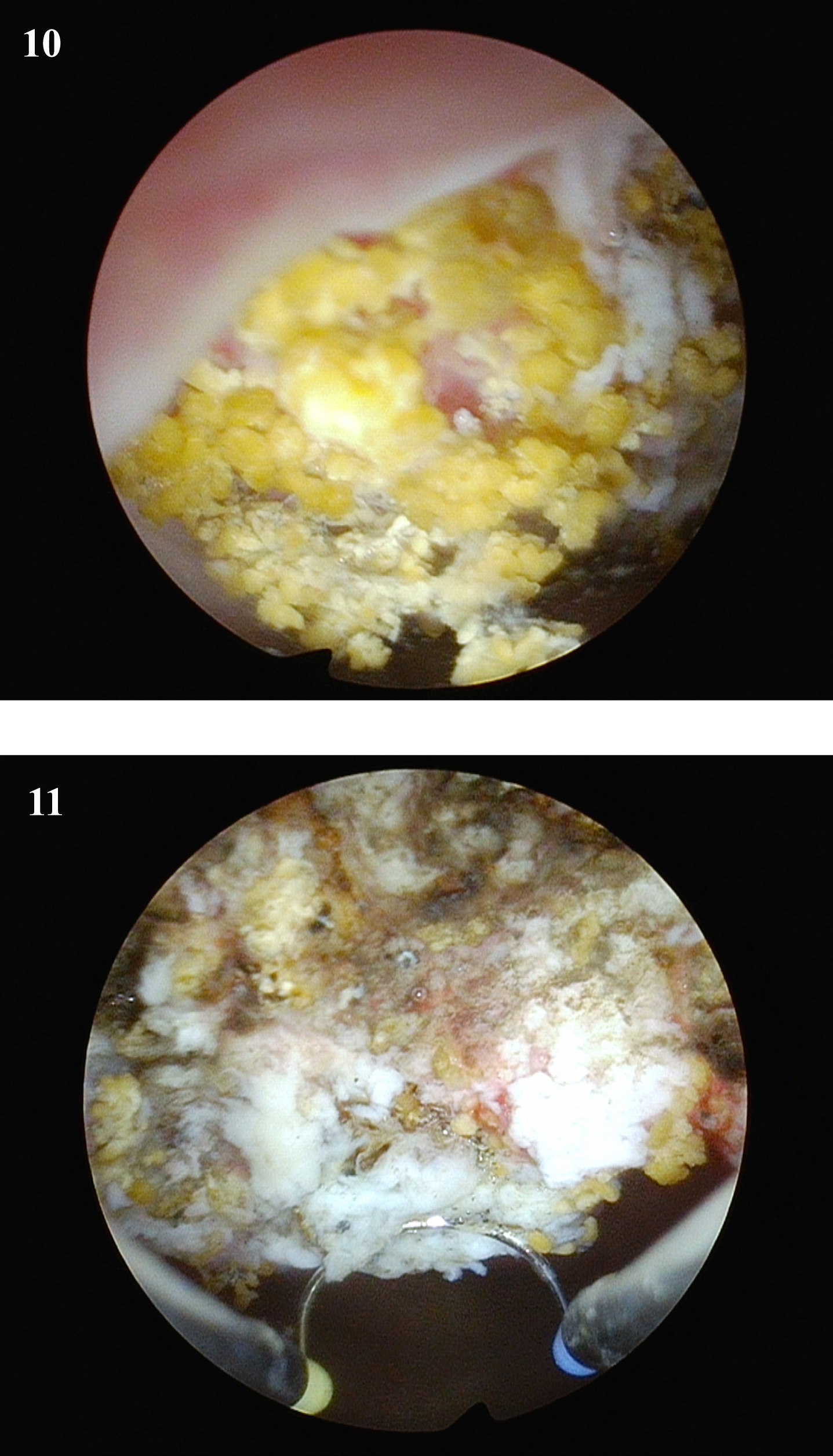
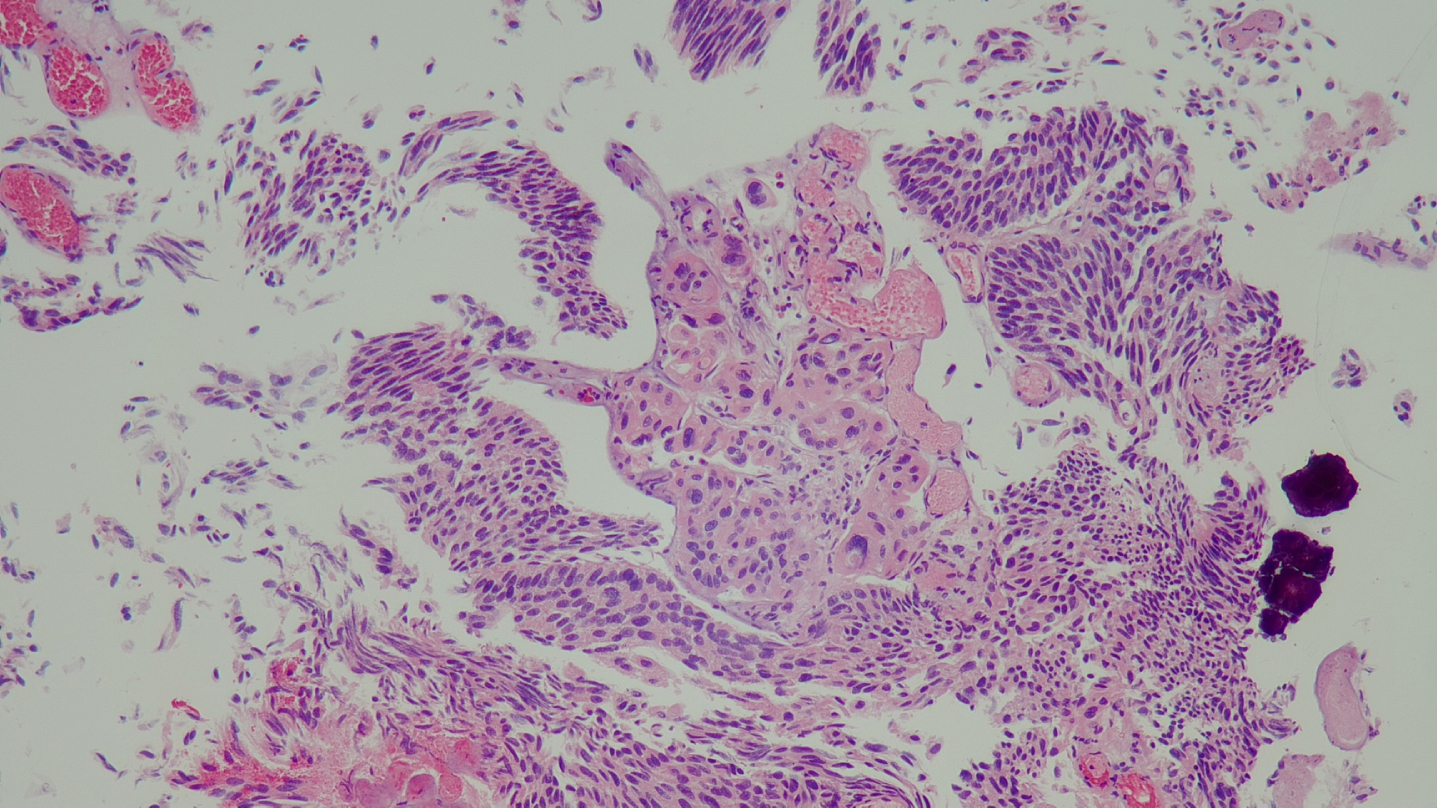
Fig. 12
Histology of the high grade urothelial carcinoma with minimal invasion of the lamina propria.
I saw him as a second opinion. He was advised to undergo induction systemic cisplatin based chaemotherapy followed by a radical cystoprostatectomy. He was adamant that he did not want to have his bladder removed. In order to evaluate whether he might be a candidate for bladder preservation I performed a TUR BT and the pathology re resected prior area of tumor revealed high grade papillary urothelial carcinoma confined to the urothelium TAa and carcinoma in situ (CIS). The rest of the bladder was normal. Muscle was present in the specimen and there was no invasion. I indicated to this patient that it would still be appropriate to proceed with chemotherapy followed by a radical cystoprostatectomy and urinary diversion. Since again wanted a bladder preservation approach. We decided to initiate his treatment with systemic chemotherapy with the plan that if he had a good response, we would discuss radiation, observation or removal of the bladder. He was given four cycles of gemcitabine and cisplatin. Chemotherapy was completed December 2020.
The patient had a flexible cystoscopy in November 2020 after two cycles to assess initial response and the bladder was normal and urinary cytology was normal. Imaging of the chest, abdomen and pelvis was normal. The next cystoscopy was January 2021 and was normal. In April 2021 cystoscopy was negative however the cytology indicated atypical cells suspicious for bladder cancer.
In April 2021 transurethral resection of areas of erythema revealed focal carcinoma in situ (CIS). He was given a six week course of BCG. Subsequent cystoscopies and cytology in July 2021, March 2022, and November 2022 were all normal.
In April 2023 he remained asymptomatic however flexible cystoscopy revealed a 4 to 5 centimeter solitary exophytic papillary tumor in the anterior wall of the bladder from the 11 to one o’clock position. A CT scan identified the tumor. The bladder outline was normal. An attempt at a TUR BT was made in May 2023. I was able to identify the large papillary tumor with the 70-degree lens but once the bladder began to fill even with this lens I was unable to see the tumor which was located at the anterior bladder neck. My impression was that the tumor was Ta or possibly T1. I then placed a resectoscope with a thirty-degree lens and could see the tumor even with complete relaxation and suprapubic pressure. Because I could see the tumor with the 70-degree lens I used a bugby electrode and began cauterizing the tumor but it was evident that the size of the tumor was too great and I could not remove much of the tumor by this approach. His obesity and the tumor location prevented a standard TURBT. I discontinued the procedure and weighed the options.
I thought there were a few options. Since the patient developed a new tumor despite chemotherapy and later BCG it is likely he will continue to develop urothelial carcinoma and thus I would try to convince him to undergo a cystoprostatectomy and urinary diversion. He continued to decline this option.
The second possibility might be the use of a flexible cystoscope with a laser. Although this might eradicate some or all of the tumor I would not have pathology and if there were bleeding it would be difficult to cauterize this area.
Lastly, I entertained a cystotomy and removal of the tumor however this would risk spilling tumor cells in the pelvis and more importantly if a subsequent cystectomy was required it would make it somewhat more difficult.
I was interested to see if others had suggestions and I presented this case via e mail as detailed above. Trinity Bivalacqua replied that in a similar scenario in a few cases he performed a perineal urethrostomy to reach the anterior bladder in obese patients and it worked for him. He left his patients with a perineal urethrostomy. I thought this suggestion was reasonable. Two weeks later I performed a perineal urethrostomy and with this approach I was able to place a resectoscope and perform what appeared to be a complete resection. The pathology was high grade urothelial cancer with focal lamina propria invasion. No muscle was present in the specimen. He received one post operative dose of intravesical gemcitabine and two weeks after the TUR BT he started BCG which has just been completed.
The story is far from over but the perineal urethrostomy was a successful approach for this man’s tumor resection. The urethral opening was closed at the end of the procedure and the catheter remained for two weeks. He is voiding well and there has been no difficulty placing a catheter for the BCG instillation. If he recurs with high grade Ta or CIS systemic immunotherapy will be an option if he persists in resisting a cystectomy.
All comments will be appreciated.
INFORMED CONSENT
Written informed consent for publication was obtained from the patient.
ETHICAL CONSIDERATIONS
The author has institutional review board approval for reviewing bladder cancer cases for outcome (MHS.2020.026).
CONFLICT OF INTEREST
Nothing to disclose.

